科学家们有了非凡的成功治疗癌症的新疫苗,他们认为可能与疾病战斗的“游戏规则”。他们已经研究出如何教人体的免疫系统识别肿瘤细胞,从而使患者被准备消灭肿瘤。
在一个案例中只有周住一个美国女人被清除了先进的血液肿瘤。她仍然是三年后还活着,和她的医生说她不是一个一次性的。
英国的研究人员正在研究一个相关的方法。这两种方法都涉及T细胞,抗感染,并让他们认识到癌细胞表面上的一个特殊标签的能力,称为WT1蛋白。本研究对白血病患者进行了。但科学家们希望他们的疫苗最终将被用来对抗许多类型的癌症,包括乳腺癌,肠癌和前列腺–细胞倾向于在其表面有WT1。甚至有人在讨论一个普遍的癌症疫苗中的一些科学家,虽然研究者自己认为这是不可能的。
在过去的三年里,专员Guenther海棠,在纽约纪念斯隆-凯特林癌症中心,与T细胞治疗15浆细胞性白血病患者学会识别癌症。这种疾病可以用化疗药物治疗但它往往喜欢继续返回。15将模具内的正常治疗几个月了。但随着他的政权,发现大约一半的木瓜博士还活着。他说:“我强烈地感到这是一个改变游戏。在治疗之前,我对这些患者说,他们对我说:“我没有选择,让我们试试这个。”他们有非常有限的寿命。一年后,他们叫我工作,说他们太忙没有时间见我。这是真的。”
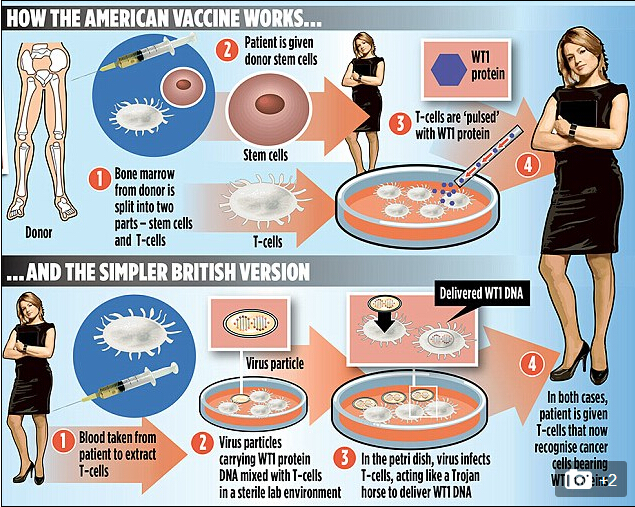
其治疗包括从供体取骨髓,分离成干细胞和T细胞。
病人接受了干细胞的直线距离,但T细胞是敏感的WT1基因在实验室暴露他们的蛋白片段。T细胞然后给病人在一系列注射过几个月。DR海棠的第一个病人,平面设计师鲁思莱西,64行的程序,2012是病后复发和化疗,她昏迷后。但在接受干细胞和四细胞的剂量,她的癌症降低到检测不到的水平。医生说看到她海棠健康良好,完全缓解”显然不平凡的经历”。
在英国的研究,LED的艾玛-莫里斯–一此时在伦敦大学学院和皇家自由医院,从20例T细胞急性髓系白血病或慢性粒细胞白血病是要被提取,插入DNA所以他们承认WT1,然后再放回去。“大多数人的免疫细胞不能识别肿瘤细胞,这是一个以应对疾病的主要问题,”莫里斯博士解释说。“我们有转基因的患者的免疫细胞,所以他们开发的WT1蛋白的受体,使他们认识到白血病细胞更好。”一个病人已经被注入含有转基因的T细胞,有些细胞正在准备。DNA转移到T细胞使用“虚拟”的病毒,不会造成感染。然后这些提供图纸建造的WT1基因表达的受体。在短期内,医生看看这些超免疫细胞将强大到足以阻止白血病患者化疗后复发。
但科学家们也希望这个方法可以帮助治疗一系列的其他癌症。莫里斯博士,他的研究与教授Hans施特劳斯被慈善白血病和淋巴瘤的研究和政府机构资助的弹弓,说:“我们可以使用它在卵巢癌,乳腺癌,前列腺癌和结肠癌患者也。”她说的方法应该产生比化疗副作用少和提供长期的保护比药物,这是从在数天或数周的身体,因为免疫细胞具有“记忆”,坚持在案件的威胁重新出现低水平。希望的是,转基因T细胞会与癌症,莫里斯博士说,“如果再需要乘以–像军队准备复活”。
Is this a miracle cancer vaccine? Scientists hail breakthrough treatment as a 'game changer'
Scientists are having extraordinary success treating cancer with new vaccines they believe could be a ‘game-changer’ in the battle against the disease.They have worked out how to teach the body’s immune system to identify cancer cells, allowing patients to be primed to destroy cancer.In one case an American woman given just weeks to live was cleared of advanced blood cancer. She is still alive three years later, and her doctor says she is not a one-off.
British researchers are now working on a related approach.
Both methods involve taking T-cells, which fight infection, and giving them the ability to recognise a special tag on the surface of cancer cells, called the WT1 protein.The research is being carried out on patients with leukaemia. But the scientists hope their vaccines will eventually be used to fight many types of cancer, including that of breast, bowel and prostate – whose cells tend to have WT1 on their surfaces.
There is even talk of a ‘universal cancer vaccine’ among some scientists, although the researchers themselves believe that is unlikely.Over the past three years, specialist Guenther Koehne, of the Memorial Sloan Kettering Cancer Center in New York, has treated 15 plasma cell leukaemia patients with T-cells taught to recognise cancer.The disease can be treated with chemotherapy-like drugs but it tends to keep returning. All 15 were expected to die within months given normal treatment. But following his regime, Dr Koehne revealed ‘about half’ were still alive.
He said: ‘I strongly feel this is a game-changer. Before treatment, I talked to these patients and they said to me: “I have no choice, let’s try this.” They had extremely limited life expectancy. A year later, they call me from work and say they are too busy to see me. That’s really happening.’His treatment involves taking bone marrow from a donor and splitting it into stem cells and T-cells.The patient receives the stem cells straight away but the T-cells are sensitised to WT1 in the lab by exposing them to fragments of the protein. The T-cells are then given to the patient in a series of injections over several months.
Dr Koehne’s first patient, graphic designer Ruth Lacey, 64, underwent the procedure in 2012 after being so ill following a relapse and intensive chemotherapy that she was ‘comatose’.But after receiving the stem cells and four T-cell doses, her cancer was reduced to undetectable levels. Dr Koehne said that seeing her ‘in good health and in complete remission’ was ‘clearly an extraordinary experience’.
In the British study, led by Dr Emma Morris – a haematologist at University College London and the Royal Free Hospital, T-cells from up to 20 patients with acute myeloid leukaemia or chronic myeloid leukaemia are to be extracted, inserted with DNA so they recognise WT1, and then put back again.‘Most people have immune cells which can’t recognise cancer cells, which is one of the major problems with tackling the disease,’ Dr Morris explained. ‘We have genetically engineered patients’ immune cells so they develop receptors for the WT1 protein, making them much better at recognising leukaemia cells.’
One patient has already received an infusion containing genetically engineered’ T-cells and there are others whose cells are being prepared. The DNA is transferred into the T-cells using a ‘dummy’ virus that does not cause an infection. These then provide the blueprint to build the WT1 receptor.In the short term, doctors are looking to see if these super-immune cells will be powerful enough to stop leukaemia patients from relapsing after chemotherapy.But scientists also hope this approach might work to help treat a range of other cancers too.
Dr Morris, whose research with Professor Hans Stauss has been funded by the charity Leukaemia and Lymphoma Research and government body Catapult, said: ‘We could potentially use it in ovarian cancer, breast cancer, and patients with prostate or colon cancer too.’
She said the approach should produce less side effects than chemotherapy and provide longer-term protection than drugs, which are flushed out of the body in days or weeks, because immune cells have a ‘memory’, persisting at low levels in case a threat re-emerges.
The hope is that the genetically engineered T-cells will do this with cancer, said Dr Morris, ‘multiplying again if needed – like an army ready to be reactivated’.
However, Dr Kat Arney of Cancer Research UK, struck a note of caution: ‘These treatments are still in the early stages of clinical trials, and although some people have had great responses, they haven’t worked for everyone.’



